A Ray Peat’s Newsletter discussing some aspects of Insomnia is below in its entirety.
All discussions with Ray Peat notes and ideas, as well as the content above his Newsletter article below are based on my own opinions and interpretations of my notes of him and what I have found useful for my own use as well as from feedback from many, many, many, many others.
This is not intended as advice, medical, legal or otherwise, and is to be used solely for educational purposes. See Program Agreement for further disclaimers and release of liability.
Dear People,
Countless numbers of people have found enormous pain relief, safely, using cannabis. We hear about others who have successfully healed their cancers. To my and the entire industry’s knowledge, no one has ever died from using just cannabis. They might have had a terrible, not-soon-forgotten emergency room experience. But they haven’t died. Before the 1920’s-30’s, it was regularly prescribed in small amounts for pain and nervous disorders by family physicians. In the 30’s it became demonized by the Rockefellers and the nascent pharmaceutical industry, eventually making cannabis so illegal and propagandized as evil, people were jailed for the rest of their lifetimes just for having the tiniest amount in their possession. However, it must be used responsibly and with mindful purpose. Some cancers it might aggravate instead of heal. Some people have allergic reactions of various types using cannabis.
So, you see all the disclaimers scattered around my cannabis topics. I hear you. Many are in so much pain, are desperate for relief, and have been around the medical establishments’ merry-go-round so many times that the disclaimers no longer matter. But here on this site, please know that in any of my cannabis topics as you review them and might start doubting again, hold your despair at bay a bit. I want to let you know that even if cannabis also ends up being not for you, this site is loaded with tons of alternatives that so many others have successfully used to reduce their pains WITHOUT any cannabis at all, or with just the slightest amount one time a day. I so encourage you to continue to explore the rest. Perhaps you too will be one of those truly free from all the drugs! Please give yourself a chance.
Solving chronic insomnia is often one of the key reasons many people want to try cannabis of any kind.
The many commercial (even the “all natural” various herbs, or main ingredient melatonin, a dangerous item) and pharmaceutical potions advertised everywhere attest to this long time and growing issue.
I myself have all too often been in this place. It’s frustrating, pitying, can be frightening to lay down to bed so exhausted and wanting to slip into the steady healing “deep sleep unconscious” where the “night can give back more than the day takes away” (L.). But 2 hours, 4 hours, an entire 6-8 hour “night” grants no such repose.
Though I think insomnia is even more insidious in these modern days, even in the early 1930’s Eleanor Roosevelt talked of what she recommended for insomnia in her advice column she then daily wrote to the American people.
She suggested that when we can’t fall asleep to do what we can to lie quietly in rest for our hours and think good and positive thoughts rather than getting up in the middle of the night in frustration to go read, or clean the house…
Well. Might have worked for her! With all she accomplished, she said she only ever needed 4 hours of sleep a night.
Some of us need more than 4 hours. And if we are otherwise in pain from our malady, our injuries, then the 4 hours, or 6 hours or 8 hours lying in uncomfortable and unforgiving repose can additionally just be torture as we try to calm down searing or aching or sharp this or that.
But I still give Eleanor’s idea some credence. With all else failing, it has worked every now and then for me. I would think all was lost and would imagine the next day sleep-walking through as if in jet-lag—but when I’d do what I could to just stay put, as bad as the sleep session, the next day always ended up being “normal”. And that next night’s sleep then usually happened ok.
But I also think there is no one solution for everyone or even for most. And no one solution for anyone with day to day insomnia. I think the solutions that are there come in complexity, in using several ideas and solutions in combination.
So here are some additional options that have worked from time to time for me and for others when visited by insistent insomnia:
- Remove ALL wi-fi, bluetooth and cellular devices, all electronics from your sleep room. Every cell phone, tablet, wi-fi computer, smart device, smart watch, EVERY wi-fi and signaling device. Every “Nest”, or “Alexa”, all of it. Shield the interior walls that are behind exterior smart utility meters with special blockers or EMF blocking paint. Use hardwire “cat-5” regular “broadband” type wires with adapters for every device to be hardwired instead of using wi-fi, but still keep it all out of your sleeping area. In the sleep area remove all these items as far away as possible, or shield any of them in faraday bags that you can. The wi-fi, especially the new 5G signals, but ALL of it, is a constant bombardment of disruptive signaling damaging our brains, tissues, our own body electromagnetics, they are high endocrine disruptors and cause a HUGE amount of insomnia these days as well as headaches, bloody noses, autoimmune symptoms. Keep all regular electronics also as far away from your bed as possible. Even electrical (or worse, wi-fi) clocks need to go. Smart TVs not only are highly EMF bodily disruptive, they emit brain entrainment, hypnosis programmings that can damage pure sleep. A more complete interview with an expert about this problem can be found here.
- Stay put in your sleeping area and shift as much as you can to whatever position is the least painful. Do slow, regular, belly breathing counting to 5 for every inhale, count 5 for every hold of the breath, count 5 for every exhale.
- And then starting with focusing on the toes on your feet and little by little moving up and across your body, begin to relax each part of your body as much as possible, in the greatest detail your mind can imagine. Move up the body little by little until you finally imagine relaxing every muscle of your face from your chin, lips, your teeth, your nose, your eyebrows, your ears, and your forehead. And continue the very slow breathing.
- Comfortable in your bed, listen to a quiet, soothing nighttime meditation (from a WIRED device, not wireless).
- Invest in the best, non-toxic and supportive bed and bedding you can afford. If you need to purchase pieces of a system only as you can afford them, go for the non-toxic sheets, blankets and pillows first. Then get a supportive pillow system. Then some kind of cushion top. I have an article here about the best bed to date I’ve found for scoliosis sufferers, those with fibromyalgia and some back injuries. Stay away from the toxic artificial materials, the no-iron polyester garbage used as bed coverings, the hot, the off-gassing, the stiff foam that takes forever to conform, the inner springs. Breathing in those poisons for hours at a time certainly does no favors for a body trying to fall into healing, deep and refreshing real sleep.
- Change what you eat during the day to ONLY eat real foods. Be diligent to particularly eat no flour, or flour substitute foods. Eat only foods chosen to be as clean as possible from glyphosate poisons. For me, if any of my (organic, but still could be poisoned) potatoes, fruits or carrots might be suspect of glyphosate contamination, or if I joined someone for a meal away from my particular foods, I can almost guarantee partial or whole sleepless nights. Some of the “labeled organic” produce foods purchased from the Walmart I have imagined have made me sick as well as sleepless. I believe those particular purchases were probably not as organic as I’d like to think!
- Run a noise-less air purifier in your sleeping area (as far away from your bed as possible because of the EMF any running electrical machine will also give off).
- Be in bright light all the way until bed but then use black-out coverings over the windows and sleep in darkness.
- Some find sleeping in a cool room more helpful, around 65 degrees F.
- Set up a quiet space for sleeping. If regular background noise is constant and disruptive, find a white noise machine and see if running that in the background helps (as far away from your bed as you can make it).
- Get enough natural light from outside during each day. For most people that’s at least about 10 minutes of safe sunlight twice a day or more—with light in the eyes, no sunglasses, no hat. Keep high-lumen room lighting on until sleep time. Use a balanced, high color rendering (90 or higher CRI, such as halogen light bulbs technology) light source with a lean towards the more “warm” light that used to be generated by the 100 watt incandescent bulbs. Remove any source of blue light from your environment. Remove ANY LED lightbulbs. Even the “warm” versions give off microwave tech flicker and unbalanced blue light. Wear blue-light-blocker eyeglasses as part of your prescription or just off-the-shelf blue light blocking glasses for any blue light from televisions (turn those spying tvs off in any case!—watch programs from a computer monitor instead). Run the IRIS blue-light-blocker app on any of your screen devices. Make sure ANY “blue light” or “daylight” type light bulbs in your environment are replaced.
- Keep the same sleep time and length of hours slept consistent and the same each day. Keep the same sleep schedule even for your weekend or days-off days.
- Remove as much scent (perfumes, fragrances) from your sleeping area as possible. Any shampoos, soaps, lotions, hair products, salves that have any fragrance, even if these are labeled as natural, organic essential oils designed for relaxation, like lavender. These scents bypass any of the brain discernment or reasoning filters to be interpreted directly by the emotional and memory brain, the limbic part of the brain. These scents could trigger all kinds of unpleasant or pleasant memories or immediate emotions of all kinds. These fragrances of any kind can also directly affect a person’s physiology, positively or negatively. They can trigger negative immune responses. They can be endocrine (thyroid) disrupters. Various scents have been known to even cause seizures in some.
- For supplements that could be helpful solving chronic insomnia, my notes with Peat suggest thyroid supplementation is often needed with high protein, salty broth (melted, dissolved, warm gelatin with a bit of salt), a bit of sugar (or orange juice with a bit of salt) before going to bed. I note that if you are getting up during the night with insomnia, eating a bit of these foods can help correct this.
- Those nights when the scoliosis or arthritis pain overtakes me, a bit of aspirin just before sleep has been an amazing supplement for me, sometimes allowing me to get into deep sleep really within a few minutes if my food has been ok for awhile.
- Here is another Peat idea that can help. I’ve used the hot shower before sleep idea myself. It seems to work best if I don’t stay too long in the heat, just enough to “get warm”.
“Increased body temperature improves sleep, especially the deep slow wave sleep. A hot bath, or even warming the feet, has the same effect as thyroid in improving sleep. Salty and sugary foods taken at bedtime, or during the night, help to improve the quality and duration of sleep. Both salt and sugar lower the adrenalin level, and both tend to raise the body temperature.”—Ray Peat. Newsletter: Thyroid, insomnia, and the insanities: Commonalities in disease
And as for cannabis, it has pros and cons as a sleep aid. I would only try it if you have completely banned all wi-fi/cellular/bluetooth/electrical devices from your sleep area and have severe pain that is not relieved enough by aspirin, thyroid, protein, and real food for you to get good, deep and healing sleep.
Most of the cannabis products are fraudulent. Some cause wakefulness instead. Some of it will knock you out but not give the real, deep, healing sleep.
- Most people are kept awake with small doses of (less than 100-200 mg) CBD-rich or CBD-only products. A THC-rich product is usually needed. If you decide to try CBD, experiment with higher doses if the small doses do not work. As well, I suggest you purchase a well known, reputable brand of CBD to try. Most of the CBD products are lacking any CBD when tested and instead poisoning you with the other additives in the product.
- Using CBN (a cannabinoid from degraded THC) is highly sedative and I think though a person feels like they “fell asleep”, they might not really be reaching that deep REM sleep needed for healing. I would suggest avoiding it.
- Many people with pain that can’t all be solved by aspirin, and the insomnia caused mostly by the pain after cleaning up the food and supplements, find success in consuming about a 15-20 mg dose of THC-rich product, either inhaling it or by using the Recipe or similar.
- Most people find the best success banning all EMF devices from their sleep area, cleaning up their food and few supplements, beginning a reliable thyroid supplement, upgrading their bedding system to a very natural as possible one, and using aspirin just before bed.

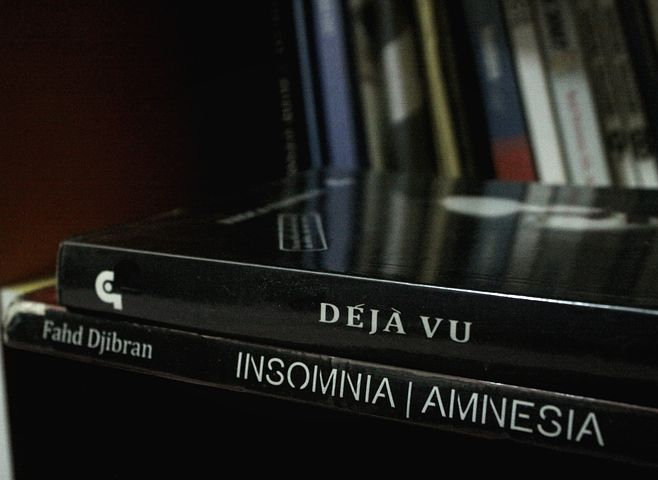
A R T I C L E
Thyroid, insomnia, and the insanities: Commonalities in disease
SOME FACTORS IN STRESS, INSOMNIA AND THE BRAIN SYNDROMES:
Serotonin, an important mediator of stress, shock, and inflammation, is a vasoconstrictor that impairs circulation in a great variety of circumstances.
Stress impairs metabolism, and serotonin suppresses mitochondrial energy production.
Stress and shock tend to increase our absorption of bacterial endotoxin from the intestine, and endotoxin causes the release of serotonin from platelets in the blood.
Schizophrenia is one outcome of stress, both cumulative and acute. Prenatal stress commonly predisposes a person to develop schizophrenia at a later age.
Serotonin’s restriction of circulation to the uterus is a major factor in toxemia of pregnancy and related complications of pregnancy.
Hypothyroidism increases serotonin activity in the body, as it increases estrogen dominance.
Estrogen inhibits the enzyme monoamino oxidase (MAO), and is highly associated with increased serotonin activity. Progesterone has the opposite effect on MAO.
The frontal lobes of the brain are hypometabolic in schizophrenia. Serotonin can cause vasoconstriction in the brain.
Serotonin release causes lipid peroxidation.
Schizophrenics have high levels of lipid peroxidation.
Antioxidants, including uric acid, are deficient in schizophrenics.
Therapies which improve mitochondrial respiration alleviate the symptoms of schizophrenia.
Energy depletion leads to brain atrophy, but with normal stimulation and nutrition even adult brains can grow.
Schizophrenics and depressed people have defective sleep.
Increasing the body’s energy level and temperature improves the quality of sleep.
================
Everyone is familiar with the problem of defining insanity, in the case of people who plead innocent by reason of insanity. The official definition of insanity in criminal law is “the inability to tell right from wrong.” Obviously, that can’t be generalized to everyday life, because any sane person realizes that certainty is impossible, and that most situations, including elections, offer you at best the choice of “the lesser of two evils,” or the opportunity to “do the right thing,” and to “throw your vote away.” People who persist in doing what they know is really right are “eccentric,” in the sense that they don’t adapt to society’s norms. In a society that chooses to destroy ecosystems, rather than adapting to them, the question of sanity should be an everyday political issue.
The use of medical terms tends to give authority to the people who are in charge of defining the terms, and it can give the impression of objectivity when there really isn’t any scientific validity behind the terms. In their historical senses, “crazy” (flawed) and “insane” (unsound) are probably more objective terms than the medically-invented terms, dementia praecox (premature idiocy) or schizophrenia (divided mind).
“Odd Speech” is one of the dimensions used in the diagnosis of insanity. I am reminded of William Wordsworth’s dismissal of William Blake as insane after failing to understand some of Blake’s poems–Wordsworth was conventional enough to become England’s Poet Laureate, and to his limited perspective, Blake’s clear verses were incomprehensibly odd.
Whenever a trusted government employee decides to blow the whistle on criminal activities, his agency invariably puts out the information that this now discharged employee is psychologically unbalanced. Dissent, in other words, is easy to dispose of by psychiatric tainting.
If we are going to speak of mental impairment, then we should have objective measures of what we are talking about. Blake unquestionably could do anything better than Wordsworth, because he was neither stupid nor dishonest, and it’s almost a rule that ordinary employees are more competent than the administrators who evaluate their work. Objective standards of mental impairment would be more popular among patients than among diagnosticians, judges, and lawmakers.
In a famous test of the objectivity of diagnosis, a filmed interview with a patient was shown to British and U.S. psychiatrists. 69% of the Americans diagnosed the patient as schizophrenic, but only 2% of the British psychiatrists did.
The strictly medical/psychological definition of insanity is still, despite the existence of the International Classification of Diseases, and in the U.S. the Diagnostic and Statistical Manual, which enumerate a large number of “mental disorders,” a crazily indefinite grouping of symptoms, and hasn’t made diagnosis more objective.. For example, in the last 30 years autism has been separated from childhood schizophrenia, but now the tendency is for both of them to be called developmental brain disorders. Both schizophrenia and autism are now often described in terms of a “spectrum of conditions,” which hardly matters, since they are not understood in terms of cause, prevention, or cure.
The problem is in the history of psychosis as a medical idea. About 100 years ago, attempts were made to classify psychoses by their symptoms, unifying a great variety of old diagnostic categories into two groups, manic-depressive mood disorders, and “dementia praecox,” or schizophrenia, which (as indicated by its name, premature dementia) was considered to be progressive and incurable. Several kinds of mental disorder were found to have clear causes, including vitamin deficiencies and various poisons and infections, but the idea of a certain thing called schizophrenia still persists.
The unitary concept of psychosis grew up in a culture in which “endogenous insanity” was a “hereditary taint,” that for a time was “treated” by imprisonment, and that more recently has been treated with sterilization or euthanasia to eliminate the “insanity genes.”
The idea that the disease is “in the genes” now serves the drug industry well, since they offer chemicals that will correct the specific “chemical error.”
Not all psychiatrists and psychologists subscribed to the idea of a unitary psychosis, defined by a variety of symptoms. A positive contribution of Freudian psychoanalysis (and its congeners and competitors) was that it made people think in terms of causes and the possibility of cures, instead of hopelessness, stigmatization, isolation and eradication. Although Freud expressed the thought that biological causes and cures would eventually be found, the profession he founded was not sympathetic to the idea of physiological therapies.
Looking for general physiological problems behind the various symptoms is very different from the practice of classifying the insanities according to their symptoms and the hypothetical “brain chemicals” that are believed to “cause the symptoms.” The fact that some patients hallucinate caused many psychiatrists to believe that hallucinogenic chemicals, interfering with nerve transmitter substances such as dopamine or serotonin, were going to provide insight into psychotic states. The dopamine excess (or serotonin deficiency) theories developed at a time when only a few “transmitter substances” were known, and when they were thought to act as very specific on/off nerve switches, rather than as links in metabolic networks. The drug industry helps to keep those ideas alive.
The idea that the brain is like a computer, and that the nerves are like wires and switches, is behind all of the theories about transmitter substances and synapses. If this metaphor about the nature of the brain and the organism is fundamentally wrong, then the theories of schizophrenia based on nerve transmitter substances can hardly be right. Another theory of schizophrenia based on the computer metaphor has to do with the idea that nerve cells’ wire-like and switch-like functions depend on their membranes, and, in the most popular version, that these all-important membranes are made of fish oil. The supporting evidence is supposed to be that the fish-oil-like fatty acids are depleted from the tissues of schizophrenics. Just looking at that point, the “evidence” is more likely to be the result of stress, which depletes unsaturated fatty acids, especially of the specified type, in producing lipid peroxides and other toxic molecules.
In one of its variations, the “essential fatty acid deficiency” doctrine suggests that a certain prostaglandin deficiency is the cause of schizophrenia, but experiments have shown that an excess of that prostaglandin mimics the symptoms of psychosis.
The drug industry’s effect on the way the organism is commonly understood has been pervasively pathological. For example, the dogma about “cell surface receptors” has sometimes explicitly led people to say that the “brain chemicals” are active only at the surface of cells, and not inside the cells.
The consequences of this mistake have been catastrophic. For example, serotonin’s precursor, tryptophan, and the drugs called “serotonin reuptake inhibitors,” and other serotonergic drugs, and serotonin itself, are carcinogenic and/or tumor promoters. Excessive serotonin is a major factor in kidney and heart failure, liver and lung disease, stroke, pituitary abnormalities, inflammatory diseases, practically every kind of sickness, at the beginning, middle, and end of life. In the brain, serotonin regulates circulation and mitochondrial function, temperature, respiration and appetite, alertness and learning, secretion of prolactin, growth hormones and stress hormones, and participates in the most complex biochemical webs. But the pharmaceutical industry’s myth has led people to believe that serotonin is the chemical of happiness, and that tryptophan is its benign nutritional precursor, and that they are going to harmlessly influence the “receptors on nerve membranes.”
A particular drug has many effects other than those that are commonly recognized as its “mechanism of action,” but when an “antidepressant” or a “tranquilizer” or a “serotonin reuptake inhibitor” alleviates a particular condition, some people argue that the condition must have been caused by the “specific chemistry” that the drug is thought to affect. Because of the computer metaphor for the brain, these effects are commonly thought to be primarily in the synapses, the membranes, and the transmitter chemicals.
The argument for a “genetic” cause of schizophrenia relies heavily on twin studies in which the frequency of both twins being schizophrenic is contrasted to the normal incidence of schizophrenia in the population, which is usually about 1%. There is a concordance of 30% to 40% between monozygotic (identical) twins, and a 5% to 10% concordance between fraternal twins, and both of these rates are higher than that of other siblings in the same family. That argument neglects the closer similarity of the intrauterine conditions experienced by twins, for example the sharing of the same placenta, and experiencing more concordant biochemical interactions between fetus and mother.
Defects of the brain, head, face, and even hands and fingerprints are seen more frequently in the genetically identical twin who later develops schizophrenia than the twin who doesn’t develop schizophrenia. Of the twins, it is the baby with the lower birth weight and head size that is at a greater risk of developing schizophrenia.
Oliver Gillie (in his book, Who Do You Think You Are?) discussed some of the fraud that has occurred in twin studies, but no additional fraud is needed when the non-genetic explanation is simply ignored and excluded from discussion. The editors of most medical and scientific journals are so convinced of the reality of genetic determination that they won’t allow their readers to see criticisms of it.
Prenatal malnutriton or hormonal stress or other stresses are known to damage the brain, and especially its most highly evolved and metabolically active frontal lobes, and to reduce its growth, relative to the rest of the body.
The standard medical explanation for the association of pregnancy toxemia and eclampsia with birth defects has been, until recently, that both mother and child were genetically inferior, and that the defective child created the pregnancy sickness. The same “reasoning” has been invoked to explain the association of birth complications with later disease: The defective baby was the cause of a difficult birth. That argument has recently been discredited (McNeil and Cantor-Graae, 1999).
Schizophrenics are known to have had a higher rate of obstetrical complications, including oxygen deprivation and Cesarian deliveries, than normal people. Like people with Alzheimer’s disease, the circumference of their heads at birth was small, in proportion to their body weight and gestational age.
Animal studies show that perinatal brain problems tend to persist, influencing the brain’s metabolism and function in adulthood.
Like the other major brain diseases, shizophrenia involves a low metabolic rate in crucial parts of the brain. In schizophrenics, “hypofrontality,” low metabolism of the frontal lobes, is characteristic, along with abnormal balance between the hemispheres, and other regional imbalances.
A very important form of prenatal stress occurs in toxemia and preeclampsia, in which estrogen is dominant, and endotoxin and serotonin create a stress reaction with hypertension and impaired blood circulation to the uterus and placenta.
The brain, just like any organ or tissue, is an energy-producing metabolic system, and its oxidative metabolism is extremely intense, and it is more dependent on oxygen for continuous normal functioning than any other organ. Without oxygen, its characteristic functioning (consciousness) stops instantly (when blood flow stops, blindness begins in about three seconds, and other responses stop after a few more seconds). The concentration of ATP, which is called the cellular energy molecule, doesn’t decrease immediately. Nothing detectable happens to the “neurotransmitters, synapses, or membrane structures” in this short period; consciousness is a metabolic process that, in the computer metaphor, would be the flow of electrons itself, under the influence of an electromotive force, a complex but continuous sort of electromagnetic field. The computer metaphor would seem to have little to offer for understanding the brain.
In this context, I think it’s necessary, for the present, to ignore the diagnostic details, the endless variety of qualifications of the idea of “schizophrenia,” that fill the literature. Those diagnostic concepts seem to tempt people to look for “the precise cause of this particular subcategory” of schizophrenia, and to believe that a specific drug or combination of drugs will be found to treat it, while encouraging them to ignore the patient’s physiology and history.
If we use the standard medical terms at all, it should be with the recognition that they are, in their present and historical form, not scientifically meaningful.
The idea that schizophrenia is a disease in itself tends to distract attention from the things it has in common with Alzheimer’s disease, autism, depression, mania, the manic-depressive syndrome, the hyperactivity-attention deficit syndrome, and many other physical and mental problems. When brain abnormalities are found in “schizophrenics” but not in their normal siblings, it could be tempting to see the abnormalities as the “cause of schizophrenia,” unless we see similar abnormalities in a variety of sicknesses.
For the present, it’s best to think first in the most general terms possible, such as a “brain stress syndrome,” which will include brain aging, stroke, altitude sickness, seizures, malnutrition, poisoning, the despair brought on by inescapable stress, and insomnia, which are relatively free of culturally arbitrary definitions. Difficulty in learning, remembering, and analyzing are objective enough that it could be useful to see what they have to do with a “brain stress syndrome.”
Stress damages the energy producing systems of cells, especially the aerobic mitochondria, in many ways, and this damage can often be repaired. The insanities that are most often called schizophrenia tend to occur in late adolescence, or around menopause, or in old age, which are times of stress, especially hormonal stress. Post-partum psychosis often has features that resemble schizophrenia.
Although the prenatal factors that predispose a person toward the brain stress syndrome, and those that trigger specific symptoms later in life, might seem to be utterly different, the hormonal and biochemical reactions are probably closely related, involving the adaptive responses of various functional systems to the problem of insufficient adaptive ability and inadequate energy.
By considering cellular energy production, local blood flow, and the systemic support system, we can get insight into some of the biochemical events that are involved in therapies that are sometimes successful. A unified concept of health and disease will help to understand both the origins and the appropriate treatments for a great variety of brain stress syndromes.
The simple availability of oxygen, and the ability to use it, are regulated by carbon dioxide and serotonin, which act in opposite directions. Carbon dioxide inhibits the release of serotonin. Carbon dioxide and serotonin are regulated most importantly by thyroid function. Hypothyroidism is characterized by increased levels of both noradrenalin and serotonin, and of other stress-related hormones, including cortisol and estrogen. Estrogen shifts the balance of the “neurotransmitters” in the same direction, toward increased serotonin and adrenalin, for example by inhibiting enzymes that degrade the monoamine “neurotransmitters.”
When an animal such as a squirrel approaches hibernation and is producing less carbon dioxide, the decrease in carbon dioxide releases serotonin, which slows respiration, lowers temperature, suppresses appetite, and produces torpor.
But in energy-deprived humans, increases of adrenalin oppose the hibernation reaction, alter energy production and the ability to relax, and to sleep deeply and with restorative effect.
In several ways, torpor is the opposite of sleep. Rapid eye movement (REM), that occurs at intervals during sleep and in association with increased respiration, disappears when the brain of a hibernating animal falls below a certain temperature. But torpor isn’t like “non-REM” deep sleep, and in fact seems to be like wakefulness, in the sense that a sleep-debt is incurred: Hibernating animals periodically come out of torpor so they can sleep, and in those periods, when their temperature rises sharply, they have a very high percentage of deep “slow wave sleep.”
Although it is common to speak of sleep and hibernation as variations on the theme of economizing on energy expenditure, I suspect that nocturnal sleep has the special function of minimizing the stress of darkness itself, and that it has subsidiary functions, including its now well confirmed role in the consolidation and organization of memory. This view of sleep is consistent with observations that disturbed sleep is associated with obesity, and that the torpor-hibernation chemical, serotonin, powerfully interferes with learning.
Babies spend most of their time sleeping, and during life the amount of time spent sleeping decreases, with nightly sleeping time decreasing by about half an hour per decade after middle age. Babies have an extremely high metabolic rate and a stable temperature. With age the metabolic rate progressively declines, and as a result the ability to maintain an adequate body temperature tends to decrease with aging.
(The simple fact that body temperature regulates all organic functions, including brain waves, is habitually overlooked. The actions of a drug on brain waves, for example, may be mediated by its effects on body temperature, but this wouldn’t be very interesting to pharmacologists looking for “transmitter-specific” drugs.)
Torpor is the opposite of restful sleep, and with aging, depression, hypothyroidism, and a variety of brain syndromes, sleep tends toward the hypothermic torpor.
An individual cell behaves analogously to the whole person. A baby’s “high energy resting state” is paralleled by the stable condition of a cell that is abundantly charged with energy; ATP and carbon dioxide are at high levels in these cells. Progesterone’s effects on nerve cells include favoring the high energy resting state, and this is closely involved in progesterone’s “thermogenic” effect, in which it raises the temperature set-point.
The basal metabolic rate, which is mainly governed by thyroid, roughly corresponds to the average body temperature. However, in hypothyroidism, there is an adaptive increase in the activity of the sympathetic nervous system, producing more adrenalin, which helps to maintain body temperature by causing vasoconstriction in the skin. In aging, menopause, and various stressful conditions, the increased adrenalin (and the increased cortisol production which is produced by excess adrenalin) causes a tendency to wake more easily, and to have less restful sleep.
While the early morning body temperature will sometimes be low in hypothyroidism, I have found many exceptions to this. In protein deficiency, sodium deficiency, in menopause with flushing symptoms, and in both phases of the manic depression cycle, and in some schizophrenics, the morning temperature is high, corresponding to very high levels of adrenalin and cortisol. Taking the temperature before and after breakfast will show a reduction of temperature, the opposite of what occurs in simple hypothyroidism, because raising the blood sugar permits the adrenalin and cortisol to fall.
The characteristic sleep pattern of hypothyroidism and old age is similar to the pattern seen in schizophrenia and depression, a decrease of deep slow wave sleep. Serotonin, like torpor, produces a similar effect. In other words, a torpor-like state can be seen in all of these brain-stress states. Several studies have found that anti-serotonin drugs improve sleep, and also reduce symptoms of schizophrenia and depression. It is common for the “neuroleptic” drugs to raise body temperature, even pathologically as in the “neuroleptic malignant syndrome.”
In old people, who lose heat easily during the day, their extreme increase in the compensatory nervous and hormonal adrenalin activity causes their night-time heat regulation (vasoconstriction in the extremities) to rise to normal.
Increased body temperature improves sleep, especially the deep slow wave sleep. A hot bath, or even warming the feet, has the same effect as thyroid in improving sleep. Salty and sugary foods taken at bedtime, or during the night, help to improve the quality and duration of sleep. Both salt and sugar lower the adrenalin level, and both tend to raise the body temperature.
Hypothyroidism tends to cause the blood and other body fluids to be deficient in both sodium and glucose. Consuming salty carbohydrate foods momentarily makes up to some extent for the thyroid deficiency.
In the peiodic table of the elements, lithium is immediately above sodium, meaning that it has the chemical properties of sodium, but with a smaller atomic radius, which makes its electrical charge more intense. Its physiological effects are so close to sodium’s that we can get clues to sodium’s actions by watching what lithium does.
Chronic consumption of lithium blocks the release of adrenalin from the adrenal glands, and it also has extensive antiserotonin effects, inhibiting its release from some sites, and blocking its actions at others.
Lithium forms a complex with the ammonia molecule, and since the ammonia molecule mimics the effects of serotonin, especially in fatigue, this could be involved in lithium’s antiserotonergic effects. Ammonia, like serotonin, impairs mitochondrial energy production (at a minimum, it uses energy in being converted to urea), so anti-ammonia, anti-serotonin agents make more energy available for adaptation. Lithium has been demonstrated to restore the energy metabolism of mitochondria (Gulidova, 1977).
Therapies that have been successful in treating “schizophrenia” include penicillin, sleep therapy, hyperbaric oxygen, carbon dioxide therapy, thyroid, acetazolamide, lithium and vitamins. These all make fundamental contributions to the restoration of biological energy. Antibiotics, for example, lower endotoxin formation in the intestine, protect against the induction by endotoxin of serotonin, histamine, estrogen, and cortisol. Acetazolamide causes the tissues to retain carbon dioxide, and increased carbon dioxide acidifies cells, preventing serotonin secretion.
REFERENCES
Gen Pharmacol 1994 Oct;25(6):1257-1262. Serotonin-induced decrease in brain ATP, stimulation of brain anaerobic glycolysis and elevation of plasma hemoglobin; the protective action of calmodulin antagonists. Koren-Schwartzer N, Chen-Zion M, Ben-Porat H, Beitner R Department of Life Sciences, Bar-Ilan University, Ramat Gan, Israel. 1. Injection of serotonin (5-hydroxytryptamine) to rats, induced a dramatic fall in brain ATP level, accompanied by an increase in P(i). Concomitant to these changes, the activity of cytosolic phosphofructokinase, the rate-limiting enzyme of glycolysis, was significantly enhanced. Stimulation of anaerobic glycolysis was also reflected by a marked increase in lactate content in brain. 2. Brain glucose 1,6-bisphosphate level was decreased, whereas fructose 2,6-bisphosphate was unaffected by serotonin. 3. All these serotonin-induced changes in brain, which are characteristic for cerebral ischemia, were prevented by treatment with the calmodulin (CaM) antagonists, trifluoperazine or thioridazine. 4. Injection of serotonin also induced a marked elevation of plasma hemoglobin, reflecting lysed erythrocytes, which was also prevented by treatment with the CaM antagonists. 5. The present results suggest that CaM antagonists may be effective drugs in treatment of many pathological conditions and diseases in which plasma serotonin levels are known to increase.
WMJ 1990 Nov-Dec;62(6):93-7. [Effect of inflammatory mediators on respiration in rat liver mitochondria]. Semenov VL.
Vopr Med Khim 1990 Sep-Oct;36(5):18-21 [Regulation by biogenic amines of energy functions of mitochondria]. Medvedev A.E. Biogenic amines (phenylethylamine, tyramine, dopamine, tryptamine, serotonin and spermine) decreased activities of the rotenone-insensitive NADH-cytochrome c reductase, the succinate cytochrome c reductase and the succinate dehydrogenase.
Vopr Med Khim 1991 Sep-Oct;37(5):2-6. [The role of monoamine oxidase in the regulation of mitochondrial energy functions]. Medvedev AE, Gorkin VZ.
Lik Sprava 1997 Jan-Feb;(1):61-5. [Microhemodynamics and energy metabolism in schizophrenia patients]. Kut’ko II, Frolov VM, Rachkauskas GS, Pavlenko VV, Petrunia AM. An apparent disturbance was revealed in microhaemodynamics of patients diagnosed as having schizophrenia (n = 210) which was more pronounced in continuously progredient form of the above medical condition. An increase in conjunctival indexes, polymorphic character of capillaries, decrease in numbers of capillary loops were revealed by biomicroscopy of the bulbar conjunctiva and capillaroscopy respectively. The patients showed lowering of ATP level and rise in the content of cathodic LDG4-LDG5 fractions, accumulation in blood of lactic and pyruvic acids.
Schizophr Res 1996 Oct 18;22(1):41-7. Are reduced head circumference at birth and increased obstetric complications associated only with schizophrenic psychosis? A comparison with schizo-affective and unspecified functional psychoses. McNeil TF, Cantor-Graae E, Nordstrom LG, Rosenlund T.
Schizophr Res 1993 Jun;10(1):7-14. Puberty and the onset of psychosis. Galdos PM, van Os JJ, Murray RM Department of Child and Adolescent Psychiatry, Bethlem Royal Hospital, London, UK. According to the neurodevelopmental hypothesis of schizophrenia, maturational events in the brain at puberty interact with congenital defects to produce psychotic symptoms. As girls reach puberty at a younger age than boys, we predicted that (i) females would show earlier onset of psychotic illness arising around puberty, and (ii) onset of psychosis in females would be related to menarche. Analysis of epidemiological data regarding admission to psychiatric units in (a) England over the period 1973-1986, (b) France over the period 1975`-1980, as well as examination of 97 psychotic adolescents referred to an adolescent unit over a 14 year period, supported both these propositions.
Int J Psychophysiol 1999 Dec;34(3):237-47. Timing of puberty and syndromes of schizotypy: a replication. Kaiser J, Gruzelier JH. “Active syndrome findings were confined to the male subsample with late maturing males showing higher scores on the Cognitive Failures and Odd Speech subscales than early maturers. As in the previous study, there was no relationship between a global psychosis proneness scale and maturational rate. These findings support a neurodevelopmental model of psychosis-proneness and show the importance of adopting a syndromal view.”
Am J Physiol 1978 Mar;234(3):H300-4. Potentiation of the cerebrovascular response to intra-arterial 5-hydroxytryptamine. Eidelman BH, Mendelow AD, McCalden TA, Bloom DS. Infusion of 5-hydroxytryptamine (5HT) into the internal carotid artery of normal baboons was not accompanied by alteration of gray matter cerebral blood flow. In animals pretreated with depot estrogen and progesterone (dosage equivalent to oral contraceptive preparations), infusion of 5HT produced a marked decrease in gray matter blood flow. A similar decrease in flow was obtained when the 5HT was infused with a concentrate of beta-lipoprotein. Steroid substances appear to enhance the cerebrovascular constrictor responses to 5HT. A further series of six experiments has shown that the monoamine oxidase inhibitor tranylcypromine similarly produced constrictor responses to 5HT. It is possible that the steroids, the beta-lipoprotein, and the tranylcypromine produced constrictor responses to 5HT by the same mechanism (inhibition of cerebrovascular monoamine oxidase).
FASEB J 1989 Apr;3(6):1753-9. Steroid regulation of monoamine oxidase activity in the adrenal medulla. Youdim MB, Banerjee DK, Kelner K, Offutt L, Pollard HB. “Administration of different steroid hormones in vivo has distinct and specific effects on the MAO activity of the adrenal medulla.” “As in the intact animal, we found that endothelial cell MAO activity was stimulated 1.5- 2.5-fold by 10 microM progesterone, hydrocortisone, and dexamethasone, inhibited by ca. 50% by 17-alpha-estradiol, but unaffected by testosterone.” “. . . steroid-induced changes in total cell division ([14C]thymidine incorporation) and total protein synthesis ([14C]leucine incorporation) were seen after changes in MAO A.”
J Pharmacol Exp Ther 1984 Apr;229(1):244-9 Mechanisms of specific change by estradiol in sensitivity of rat uterus to serotonin. Ichida S, Oda Y, Tokunaga H, Hayashi T, Murakami T, Kita T.
Neuroendocrinology 1983;36 (3): 235-41. Gonadal hormone regulation of MAO and other enzymes in hypothalamic areas. Luine VN, Rhodes JC. “Activities of type A monoamine oxidase (MAO), acetylcholine esterase (AChE), and glucose-6-phosphate dehydrogenase (G6PDH) were differentially altered in hormone-sensitive areas of the preoptic-hypothalamic continuum after administration of estrogen and progesterone.” “Estrogen decreased activity of MAO in the PVE of the anterior hypothalamus, pars lateralis of the ventromedial nucleus and in the Ar-ME. Acute administration of progesterone (1 h) to estrogen-treated females did not further alter estrogen-dependent changes in AChE or G6PDH; however, MAO activity in the ventromedial nucleus and Ar-ME was rapidly increased after progesterone.” “Administration of the protein synthesis inhibitor anisomycin prior to progesterone did not antagonize progesterone-dependent increases in MAO. Progesterone added in vitro to homogenates from estrogen-treated but not from untreated females increased MAO activity.”
J Neurochem 1981 Sep;37(3):640-8. Gonadal influences on the sexual differentiation of monoamine oxidase type A and B activities in the rat brain. Vaccari A, Caviglia A, Sparatore A, Biassoni R “When masculinization was prevented by neonatal administration of estradiol (E) to males, hypothalamic MAO-A and MAO-B activities increased in both control and MAO-inhibited rats.” “. . . single, high doses of steroids to adult, but not to newborn rats, did acutely affect the kinetics of MAO-A. The activity of MAO-A was also decreased by high concentrations of E or TS in vitro. The imprinting for patterns of hypothalamic MAO-A and MAO-B in the two sexes results, probably, from genetic predetermination.”
Gynecol Obstet Invest 2000;49(3):150-5. Transport and metabolism of serotonin in the human placenta from normal and severely pre-eclamptic pregnancies. Carrasco G, Cruz MA, Gallardo V, Miguel P, Dominguez A, Gonzalez C. “These findings suggest that the higher plasma-free serotonin levels observed in severe pre-eclampsia are mainly due to a reduction in MAO-A activity and not limited by the rate of serotonin uptake into the cells.”
Psychiatry Res 1989 Jun;28(3):279-88. Acetazolamide and thiamine: an ancillary therapy for chronic mental illness. Sacks W, Esser AH, Feitel B, Abbott K Cerebral Metabolism Laboratory, Nathan S. Kline Institute for Psychiatric Research, Orangeburg, NY 10962. Twenty-four chronic schizophrenic patients were treated successfully with the addition of acetazolamide and thiamine (A + T) to their unchanged existing therapies in a double-blind, placebo-controlled crossover study. Therapeutic effects were measured by the Scale for the Assessment of Positive Symptoms and the Scale for the Assessment of Negative Symptoms. Overall, 50% of the patients showed improvement on all assessment scales. No untoward effects occurred in these patients or in patients in previous studies who have been treated continuously with A + T therapy for as long as 3 years.
J Neural Transm 1998;105(8-9):975-86. Role of tryptophan in the elevated serotonin-turnover in hepatic encephalopathy. Herneth AM, Steindl P, Ferenci P, Roth E, Hortnagl H. “The increase of the brain levels of 5-hydroxyindoleacetic acid (5-HIAA) in hepatic encephalopathy (HE) suggests an increased turnover of serotonin (5-HT).”
J Neurosci Res 1981;6(2):225-36 A difference in the in vivo cerebral production of [1-14C] lactate from D-[3-14C] glucose in chronic mental patients. Sacks W, Schechter DC, Sacks S. “Previously unpublished whole-blood lactate determinations in these experiments indicated a cerebral production of much higher specific activity of [1-14C]-lactate from the D-[3-14C] glucose by mental patients.”
Ther Umsch 2000 Feb;57(2):76-80. [Antidepressive therapy by modifying sleep]. Haug HJ, Fahndrich E.
Schizophr Res 1998 Jun 22;32(1):1-8. Reduced status of plasma total antioxidant capacity in schizophrenia. Yao JK, Reddy R, McElhinny LG, van Kammen DP.
FASEB J 1998 Dec;12(15):1777-83. Increased F2-isoprostanes in Alzheimer’s disease: evidence for enhanced lipid peroxidation in vivo. Pratico D, MY Lee V, Trojanowski JQ, Rokach J, Fitzgerald GA.
Dis Nerv Syst 1976 Feb;37(2):98-103. Glucose-insulin metabolism in chronic schizophrenia. Brambilla F, Guastalla A, Guerrini A, Riggi F, Rovere C, Zanoboni A, Zanoboni-Muciaccia W.
Psychiatr Clin (Basel) 1975;8(6):304-13. Blood flow and oxidative metabolism of the brain in patients with schizophrenia. Hoyer S, Oesterreich K.
Zh Nevropatol Psikhiatr Im S S Korsakova 1977;77(8):1179-86 [Effect of lithium on the energy metabolism of nervous tissue]. Gulidova GP, Khzardzhian VG, Mikhailova NM. “Lithium (0.5–4 mM) either significantly increase, either completely normalizers the intensity of the oxidative and energy metabolism of the brain mitochondria, decreased by the influence of the blood serum of patients with manic-depressive psychosis and attack like schizophrenia.” “Processes of phosphorilation become normalized in a joint action on the mitochondria by lithium and antioxidants.” “It is assumed that an increase in the intensity of the energy metabolism is one of the mechanisms of therapeutical and prophylactic action of lithium.”
Ateneo Parmense Acta Biomed 1975 Jan-Apr;46(1-2):5-19. [Clinical significance of changes in tryptophan metabolism]. Ambanelli U, Manganelli P. “The oxidative pathway is most important of the metabolic pathway of the amino acid; the degredation of tryptophan is particularly influenced by steroid hormones and vitamins’ want. The metabolic anomalies are demonstrable both in malignant tumors (mostly in bladder cancer and Hodgkin’s disease), both during psychiatric diseases (such as depression and schizophrenia) and in the diseases of connective tissue in addition to congenital errors of the degradation of tryptophan (such as Hartnup’s disease, tryptophanuria and 3-hydroxychinureninuria).”
Acta Neurol Scand Suppl 1977;64:534-5. Blood flow and oxidative metabolism of the brain in the course of acute schizophrenia. Hoyer S, Oesterreich K.
Med Hypotheses 1994 Dec;43(6):420-35 Schizophrenia is a diabetic brain state: an elucidation of impaired neurometabolism. Holden RJ, Mooney PA.
Neuropsychobiology 1990-91;24(1):1-7. Frontality, laterality, and cortical-subcortical gradient of cerebral blood flow in schizophrenia: relationship to symptoms and neuropsychological functions. Sagawa K, Kawakatsu S, Komatani A, Totsuka S.
Schizophr Res 1989 Nov-Dec;2(6):439-48. Effect of attention on frontal distribution of delta activity and cerebral metabolic rate in schizophrenia. Guich SM, Buchsbaum MS, Burgwald L, Wu J, Haier R, Asarnow R, Nuechterlein K, Potkin S. “Analysis confirmed increased delta activity in the frontal region of patients with schizophrenia in comparison to normal controls, and a significant correlation between increased frontal delta and relative reduction in frontal lobe metabolism among patients with schizophrenia. This finding of increased delta is consistent with PET, blood flow and topographic EEG studies of schizophrenia, suggesting reduced frontal activity.”
Br J Psychiatry 1990 Feb;156:216-27. Glucose metabolic rate in normals and schizophrenics during the Continuous Performance Test assessed by positron emission tomography. Buchsbaum MS, Nuechterlein KH, Haier RJ, Wu J, Sicotte N, Hazlett E, Asarnow R, Potkin S, Guich S “When the group of schizophrenic patients was divided into deficit and nondeficit types, a preliminary exploratory analysis suggested thalamic, frontal, and parietal cortical hypometabolism in the deficit subgroup, with normal metabolism in the nondeficit patient group in those areas; in contrast, hippocampal and anterior cingulate cortical metabolism was reduced in both deficit and nondeficit subtypes. These results suggest that the limbic system, especially the hippocampus, is functionally involved in schizophrenic psychosis and that different manifestations of schizophrenia may involve different neuronal circuits.”
Psychol Med 1994 Nov;24(4):947-55. Patterns of cortical activity in schizophrenia. Schroeder J, Buchsbaum MS, Siegel BV, Geider FJ, Haier RJ, Lohr J, Wu J, Potkin SG. “Schizophrenics were significantly more hypofrontal than the controls, with higher values on the ‘parietal cortex and motor strip’ factor and a trend towards higher values in the temporal cortex. A canonical discriminant analysis confirmed that the ‘hypofrontality’ and ‘parietal cortex and motor strip’ factors accurately separated the schizophrenic group from the healthy controls.”
Schizophr Res 1996 Mar;19(1):41-53. Cerebral metabolic activity correlates of subsyndromes in chronic schizophrenia. Schroder J, Buchsbaum MS, Siegel BV, Geider FJ, Lohr J, Tang C, Wu J, Potkin SG. “The delusional cluster showed a significantly reduced hippocampal activity, while the negative symptoms cluster presented with a prominent hypofrontality and significantly increased left temporal cortex values.”
Psychiatry Res 1997 Oct 31;75(3):131-44. Cerebral glucose metabolism in childhood onset schizophrenia. Jacobsen LK, Hamburger SD, Van Horn JD, Vaituzis AC, McKenna K, Frazier JA, Gordon CT, Lenane MC, Rapoport JL, Zametkin AJ. “Decreased frontal cortical glucose metabolism has been demonstrated in adult schizophrenics both at rest and while engaging in tasks that normally increase frontal metabolism, such as the Continuous Performance Test (CPT).”. “These findings suggest that childhood onset schizophrenia may be associated with a similar, but not more severe, degree of hypofrontality relative to that seen in adult onset schizophrenia.”
Pharmacol Biochem Behav 1990 Apr; 35(4):955-62. The effects of ondansetron, a 5-HT3 receptor antagonist, on cognition in rodents and primates. Barnes JM, Costall B, Coughlan J, Domeney AM, Gerrard PA, Kelly ME, Naylor RJ, Onaivi ES, Tomkins DM, Tyers MB. “The selective 5-HT3 receptor antagonist, onansetron, has been assessed in three tests of cognition in the mouse, rat and marmoset. In a habituation test in the mouse, ondansetron facilitated performance in young adult and aged animals, and inhibited an impairment in habituation induced by scopolamine, electrolesions or ibotenic acid lesions of the nucleus basalis magnocellularis.” “In an object discrimination and reversal learning task in the marmoset, assessed using a Wisconsin General Test Apparatus, ondansetron improved performance in a reversal learning task. We conclude that ondansetron potently improves basal performance in rodent and primate tests of cognition and inhibits the impairments in performance caused by cholinergic deficits.”
Pharmacol Biochem Behav 1992 May;42(1):75-83. Ondansetron and arecoline prevent scopolamine-induced cognitive deficits in the marmoset. Carey GJ, Costall B, Domeney AM, Gerrard PA, Jones DN, Naylor RJ, Tyers MB School of Pharmacy, University of Bradford, UK. The cognitive-enhancing potential of the 5-hydroxytryptamine (5-HT) selective 5-HT3 receptor antagonist, ondansetron, was investigated in a model of cognitive impairment induced by the muscarinic receptor antagonist, scopolamine.
J Comp Physiol Psychol 1977 Jun;91(3): 642-8. Tryptophan and tonic immobility in chickens: effects of dietary and systemic manipulations. Gallup GG Jr, Wallnau LB, Boren JL, Gagliardi GJ, Maser JD, Edson PH. “Systemic injections of tryptophan, the dietary precursor to serotonin, led to a dose-dependent increase in immobility, with optimal effects being observed within 30 min after injection. Dietary depletion of endogenous tryptophan served to attenuate the duration of immobility, and a diet completely free of tryptophan, but supplemented with niacin, practically abolished the reaction. Dietary replacement served to reinstate the response.” “The data are discussed in light of evidence showing serotonergic involvement in tonic immobility.”
J Neurosci Res 1995 Feb 15;40(3):407-413. Endotoxin administration stimulates cerebral catecholamine release in freely moving rats as assessed by microdialysis. Lavicky J, Dunn AJ.
J Neurosci Res 1998 Feb 15;51(4):517-525. Lipopolysaccharide regulates both serotonin- and thrombin-induced intracellular calcium mobilization in rat C6 glioma cells: possible involvement of nitric oxide synthase-mediated pathway. Tawara Y, Kagaya A, Uchitomi Y, Horiguchi J, Yamawaki S.
Infect Immun 1996 Dec;64(12):5290-5294..Biphasic, organ-specific, and strain-specific accumulation of platelets induced in mice by a lipopolysaccharide from Escherichia coli and its possible involvement in shock. Shibazaki M, Nakamura M, Endo Y. “Platelets contain a large amount of 5-hydroxytryptamine (5HT, serotonin). Intravenous injection into BALB/c mice of a Boivin’s preparation of lipopolysaccharide (LPS) from Escherichia coli induced rapid 5HT accumulation in the lung (within 5 min) and slow 5HT accumulation in the liver (2 to 5 h later).” “A shock, which was manifested by crawling, convulsion, or prostration, followed shortly after the rapid accumulation of 5HT in the lung. On the other hand, the slow accumulation of 5HT in the liver could be induced by much lower doses of LPS (1 microg/kg or less), even when given by intraperitoneal injection.”
Life Sci 1997;61(18):1819-1827. Serotonin 5HT2A receptor activation inhibits inducible nitric oxide synthase activity in C6 glioma cells. Miller KJ, Mariano CL, Cruz WR.
Harefuah 2000 May 15;138(10):809-12, 910. [Jet lag causing or exacerbating psychiatric disorders]. Katz G, Durst R, Zislin J, Knobler H, Knobler HY. We presume, relying on the literature and our accumulated experience, that in predisposed individuals jet lag may play a role in triggering exacerbation of, or de novo affective disorders, as well as, though less convincing, schizophreniform psychosis or even schizophrenia. An illustrative case vignette exemplifies the possible relationship between jet lag following eastbound flight and psychotic manifestations.
Life Sci 1987 May 18;40(20):2031-9. Dysfunction in a prefrontal substrate of sustained attention in schizophrenia. Cohen RM, Semple WE, Gross M, Nordahl TE, DeLisi LE, Holcomb HH, King AC, Morihisa JM, Pickar D. Regional brain metabolism was measured in normal subjects and patients with schizophrenia while they performed an auditory discrimination task designed to emphasize sustained attention. A direct relationship was found in the normal subjects between metabolic rate in the middle prefrontal cortex and accuracy of performance. The metabolic rate in the middle prefrontal cortex of patients with schizophrenia, even those who performed as well as normals, was found to be significantly lower than normal and unrelated to performance. The findings point to a role of the mid-prefrontal region in sustained attention and to dysfunction of this region in schizophrenia.
Acta Psychiatr Scand 1987 Dec;76(6):628-41. Regional brain glucose metabolism in drug free schizophrenic patients and clinical correlates. Wiesel FA, Wik G, Sjogren I, Blomqvist G, Greitz T, Stone-Elander S. “Thus, the lower the metabolic rate was, the more autistic the patient. Metabolic rates were not correlated to atrophic changes of the brain. No basis for a specific alteration in frontal cortical metabolism of schizophrenics was obtained. Changes in regional metabolic rates in schizophrenia are suggested to reflect disturbances in more general mechanisms which are of importance in neuronal function.”
Chung Hua Shen Ching Ching Shen Ko Tsa Chih 1991 Oct;24(5):268-71, 316-7. [Developments observation of serum thyrohormone level in schizophrenics. Wang X. “The authors reported that abnormal levels of T4, FT4I in 16 cases patients relate to disease course and severe symptoms and suggested that the change of serum T4, FT4I in some cases was related to the disease in itself.”
Biol Psychiatry 1991 Mar 1;29(5):457-66. Multidimensional hormonal discrimination of paranoid schizophrenic from bipolar manic patients. Mason JW, Kosten TR, Giller EL.
Zh Nevropatol Psikhiatr Im S S Korsakova 1991;91(1):122-3 [Status of the thyroid gland in patients with schizophrenia]. Turianitsa IM, Lavkai IIu, Mishanich II, Margitich VM, Razhov KF. “The rise of TTH concentration represents one of the mechanisms of correction, aimed at the attainment of the physiological content of T4 at the expense of its additional output for its level in the blood serum is appreciably reduced.”
Can J Psychiatry 1990 May;35(4):342-3. Increased detection of elevated TSH using immunoradiometric assay. Little KY, Kearfott KS, Castellanos X, Rinker A, Whitley R. Using a highly sensitive immunoradiometric assay, the authors detected an increased rate of elevated thyrotropin in 2,099 patients vs 1,789 patients examined with radioimmunoassay. Closer scrutiny of mood disorder patients with elevations found confirmatory evidence of thyroid dysfunction in most.
Metabolism 1990 May;39(5):538-43. Serum thyrotropin in hospitalized psychiatric patients: evidence for hyperthyrotropinemia as measured by an ultrasensitive thyrotropin assay. Chopra IJ, Solomon DH, Huang TS.
J Nerv Ment Dis 1989 Jun;177(6):351-8. Serum thyroxine levels in schizophrenic and affective disorder diagnostic subgroups. Mason JW, Kennedy JL, Kosten TR, Giller EL Jr. “For TT4, 75% of the PS group showed a rise during recovery in contrast to 4% of the remaining groups; for FT4, 50% of the PS group showed a rise compared with 14% of the other groups.” “This study emphasizes the importance of exploring more fully the psychiatric significance of thyroxine levels within the endocrinological normal range and of doing longitudinal assessments of thyroxine and symptom changes during clinical recovery in psychiatric disorders.”
Biol Psychiatry 1989 Jan;25(1):67-74. Serum thyroxine change and clinical recovery in psychiatric inpatients. Southwick S, Mason JW, Giller EL, Kosten TR. “A strong correlation between the range values for BPRS [Brief Psychiatric Rating Scale] sum and for FT4 (p less than 0.005) and TT4 (p less than 0.001) levels indicated that change in overall symptom severity was linked to change in thyroxine levels during clinical recovery.” “These findings suggest that a “normalizing” principle underlies the relationship between clinical recovery and thyroxine levels and that both FT4 and TT4 levels within the normal range appear to have clinical significance in either reflecting or contributing to the course of a variety of psychiatric disorders and possibly having a role in pathogenesis.”
J Clin Psychiatry 1980 Sep;41(9):316-8. Myxedema psychosis–insanity defense in homicide. Easson WM.
Int J Psychiatry Med 1988;18(3):263-70. The diagnostic dilemma of myxedema and madness, axis I and axis II: a longitudinal case report. Darko DF, Krull A, Dickinson M, Gillin JC, Risch SC. “A patient with presumed chronic paranoid schizophrenia had chronic thyroiditis and Grade I hypothyroidism. Psychosis cleared following treatment with thyroid replacement.” “The differential diagnosis among hypothyroidism and primary axis I psychotic and depressive psychopathology has always been problematic.”
P R Health Sci J 1993 Jun;12(2):85-7. [Alzheimer’s disease: the untold story]. Pico-Santiago G. After considering the potential relationship between amyloid deposits and myxedematous infiltrations, the hypothesis is formulated that Alzheimer’s disease may be due to functional hypothyroidism and may thus respond to thyroid therapy.
Psychiatry Res 1998 Jul 27;80(1):29-39. Reduced level of plasma antioxidant uric acid in schizophrenia. Yao JK, Reddy R, van Kammen DP. “There is evidence of dysregulation of the antioxidant defense system in schizophrenia. The purpose of the present study was to examine whether uric acid, a potent antioxidant, is reduced in the plasma of patients with schizophrenia.” “Male schizophrenic patients with either a haloperidol treatment (n=47) or a drug-free condition (n=35) had significantly lower levels of plasma uric acid than the age- and sex-matched normal control subjects (n=34).” “In addition, the plasma levels of uric acid in patient groups were significantly and inversely correlated with psychosis. There was a trend for lower uric acid levels in relapsed patients relative to clinically stable patients. Smoking, which can modify plasma antioxidant capacity, was not found to have prominent effects on uric acid levels. The present finding of a significant decrease of a selective antioxidant provides additional support to the hypothesis that oxidative stress in schizophrenia may be due to a defect in the antioxidant defense system.”
Zh Nevropatol Psikhiatr Im S S Korsakova 1989; 89(5):108-10. [Lipid peroxidation processes in patients with schizophrenia]. Kovaleva ES, Orlov ON, Tsutsu’lkovskaia MIa, Vladimirova TV, Beliaev BS.
Zh Nevropatol Psikhiatr Im S S Korsakova 1991;91(7):121-4. [Significance of disorders of the processes of lipid peroxidation in patients with persistent paranoid schizophrenia resistant to the treatment]. Govorin NV, Govorin AV, Skazhutin SA.
Patol Fiziol Eksp Ter 1999 Jul-Sep;(3):19-22. [The biogenic amine content of rat tissues in the postresuscitation period following hemorrhagic shock and the effect of the preparation semax]. Bastrikova NA, Shestakova SV, Antonova SV, Krushinskaia IaV, Goncharenko EN, Kudriashova NIu, Novoderzhkina IS, Sokolova NA, Kozhura VL. “Early after resuscitation the trend was noted to higher LPO products concentration in plasma and serotonin in the brain stem.” “It is suggested that biogenic amines, especially serotonin system, are involved in mechanisms of postresuscitation disorders, in cerebral defects in particular, through prolongation of secondary hypoxia early after hemorrhagic shock and activation of hypothalamo-hypophyso-adrenal system late after the shock.”
Prostaglandins Leukot Essent Fatty Acids 1996 Aug;55(1-2):33-43. Free radical pathology in schizophrenia: a review. Reddy RD, Yao JK.
Schizophr Res 1996 Mar;19(1):19-26. Impaired antioxidant defense at the onset of psychosis. Mukerjee S, Mahadik SP, Scheffer R, Correnti EE, Kelkar H.
Biol Psychiatry 1998 May 1;43(9):674-9. Elevated plasma lipid peroxides at the onset of nonaffective psychosis. Mahadik SP, Mukherjee S, Scheffer R, Correnti EE, Mahadik JS.
Brain Res 1999 Aug 21;839(1):74-84. Psychological stress-induced enhancement of brain lipid peroxidation via nitric oxide systems and its modulation by anxiolytic and anxiogenic drugs in mice. Matsumoto K, Yobimoto K, Huong NT, Abdel-Fattah M, Van Hien T, Watanabe H. “The effects of diazepam and FG7142 were abolished by the BZD receptor antagonist flumazenil (10 mg/kg, i.p.). These results indicate that psychological stress causes oxidative damage to the brain lipid via enhancing constitutive NOS-mediated production of NO, and that drugs with a BZD or 5-HT(1A) receptor agonist profile have a protective effect on oxidative brain membrane damage induced by psychological stress.”
Anesteziol Reanimatol 1998 Nov-Dec; (6):20-5. [Role of hyperbaric oxygenation in the treatment of posthypoxic encephalopathy of toxic etiology]. Ermolov AS, Epifanova NM, Romasenko MV, Luzhnikov EA, Ishmukhametov AI, Golikov PP, Khvatov VB, Kukshina AA, Davydov BV, Kuksova NS, et al. Hyperbaric oxygenation (HBO) was used in the treatment of 475 patients with toxic encephalopathy (TE) developing as a result of exo- and endotoxicosis. HBO promoted correction of all components of homeostasis, decreased endotoxicosis, reduced psychopathological and neurological disorders, and promoted social adaptation.
J Neurochem 2000 Jan; 74(1): 114-24. Metabolic impairment elicits brain cell type-selective changes in oxidative stress and cell death in culture. Park LC, Calingasan NY, Uchida K, Zhang H, Gibson GE. “Abnormalities in oxidative metabolism and inflammation accompany many neurodegenerative diseases. Thiamine deficiency (TD) is an animal model in which chronic oxidative stress and inflammation lead to selective neuronal death, whereas other cell types show an inflammatory response.” “Among the cell types tested, only in neurons did TD induce apoptosis and cause the accumulation of 4-hydroxy-2-nonenal, a lipid peroxidation product. On the other hand, chronic lipopolysaccharide-induced inflammation significantly inhibited cellular dehydrogenase and KGDHC activities in microglia and astrocytes but not in neurons or endothelial cells. The results demonstrate that the selective cell changes during TD in vivo reflect inherent properties of the different brain cell types.”
Psychol Med 1976 Aug;6(3):359-69. Possible association of schizophrenia with a disturbance in prostaglandin metabolism: a physiological hypothesis. Feldberg W. Schizophrenia may be associated with increased prostaglandin synthesis in certain parts of the brain. This hypothesis is based on the following findings: (1) Catalepsy, which is the nearest equivalent in animals to human catatonia, develops in cats when prostaglandin E1 is injected into the cerebral ventricles and when during endotoxin or lipid A fever the prostaglandin E2 level in cisternal c.s.f. rises to high levels; however, when fever and prostaglandin level are brought down by non-steroid anti-pyretics which inhibit prostaglandin synthesis, catalepsy disappears as well. (2) Febrile episodes are a genuine syndrome of schizophrenia.
Zh Nevropatol Psikhiatr Im S S Korsakova 1966;66(6):912-7. [Treatment of acute schizophrenia with antibiotics, gamma-globulin and vitamins]. Neikoya M.
Prostaglandins Med 1979 Jan;2(1):77-80. Penicillin and essential fatty acid supplementation in schizophrenia. Vaddadi KS.
Psychiatr Dev 1989 Spring;7(1):19-47. Positron emission tomography in psychiatry. Wiesel FA. “Schizophrenia is the most extensively studied psychiatric disorder. Most studies have demonstrated decreased metabolic rates in wide areas of the brain. It is proposed that the metabolic changes observed in the brains of schizophrenic patients are due to a fundamental change in neuronal function.” “Bipolar depressed patients probably have a decreased brain metabolism.” “Alcohol dependent subjects with a long duration of abuse may have a decreased brain metabolism.”
Arch Gen Psychiatry 1976 Nov;33(11):1377-81. Platelet monamine oxidase in chronic schizophrenia. Some enzyme characteristics relevant to reduced activity. Murphy DL, Donnelly CH, Miller L, Wyatt RJ. “These findings suggest that the reduced MAO activity found in chronic schizophrenic patients is apparently not accounted for by nonspecific changes in platelets or platelet mitochondria.”
Exp Neurol 1997 May;145(1):118-29. Long-term reciprocal changes in dopamine levels in prefrontal cortex versus nucleus accumbens in rats born by Caesarean section compared to vaginal birth. El-Khodor BF, Boksa P. “Epidemiological evidence indicates a higher incidence of pregnancy and birth complications among individuals who later develop schizophrenia, a disorder linked to alterations in mesolimbic dopamine (DA) function. Two birth complications usually included in these epidemiological studies, and still frequently encountered in the general population, are birth by Caesarean section (C-section) and fetal asphyxia.” “At 2 months of age, in animals born by rapid C-section, steady state levels of DA were decreased by 53% in the prefrontal cortex and increased by 40% in both the nucleus accumbens and striatum, in comparison to the vaginally born group. DA turnover increased in the prefrontal cortex, decreased in the nucleus accumbens, and showed no significant change in the striatum, in the C-section group. Thus, birth by a Caesarean procedure produces long-term reciprocal changes in DA levels and metabolism in the nucleus accumbens and prefrontal cortex.” “Although appearing robust at birth on gross observation, more subtle measurements revealed that rat pups born by C-section show altered respiratory rates and activity levels and increased levels of whole brain lactate, suggestive of low grade brain hypoxia, during the first 24 h of life, in comparison to vaginally born controls.” “It is concluded that C-section birth is sufficient perturbation to produce long-lasting effects on DA levels and metabolism in the central nervous system of the rat.”
Rehabilitation (Stuttg) 1983 May;22(2):81-5 [Physical capacity of schizophrenic patients]. Deimel H, Lohmann S. “Reduced physical capacity in schizophrenic illness has been described in medical literature, but so far not been substantiated empirically. The findings of progressive bicycle ergometry confirm the assertion, with the following main results having been obtained: 1. As opposed to a matched comparison group of untrained healthy clients, the schizophrenically ill patients demonstrated significantly lower endurance levels in respect of the aerobic-anaerobic threshold. 2. Relative to the load maximum attainable highly significant differences existed between the groups. Particularly noteworthy had been early exercise termination already at submaximal loads by the schizophrenic patients. 3. The patients under study obtained values one third below standard compared to the maximum load target for untrained persons, with age and weight being taken into account.”
Folia Psychiatr Neurol Jpn 1984;38(4):425-36 Antipsychotic and prophylactic effects of acetazolamide (Diamox) on atypical psychosis. Inoue H, Hazama H, Hamazoe K, Ichikawa M, Omura F, Fukuma E, Inoue K, Umezawa Y We investigated the antipsychotic and prophylactic effects of acetazolamide (Diamox) on atypical psychosis. Acetazolamide was given to 30 patients: Type I, puberal periodic psychosis, a psychosis whose onset occurs during the period of puberty and which appears repetitively with psychosis-like condition at about the same interval as the menstrual cycle (6 cases); Type II, a) presenile atypical psychosis which initially appears in patients in their 20s or 30s accompanied by manic-depressive cycles and shows acute confusional and dreamy states in the presenile period, incurable cases (7), b) atypical psychosis, in the narrow sense, cases which show acute hallucination, delusion, confusional and dreamy states accompanied by affective symptoms (8 cases); Type III, repetitively the atypical manic and depressive states, and atypical manic-depressive psychosis, and transient changes in consciousness, refractory cases (2); Type IV, atypical schizophrenia, which is considered to be schizophrenia but shows the abnormalities in electroencephalogram and emotional disorders (7 cases). Among these cases, some extent of the therapeutic effects of acetazolamide (500-1,000 mg/day) was obtained in about 70%. The high therapeutic effects were particularly observed in Types I, II and III. It was less effective against atypical schizophrenia. Acetazolamide showed the effectiveness in 10 cases out of 13 cases to which lithium carbonate and carbamazepine were ineffective. The high therapeutic effects of acetazolamide were shown in the cases whose symptoms were aggravated at the interval of the menstrual cycle. No correlation was observed between the electroencephalographic abnormalities and the therapeutic effects. In addition, the prophylactic effects of acetazolamide on the periodic crisis were observed in 9 cases. From these results, acetazolamide was considered to have the antipsychotic and prophylactic effects on atypical psychosis. Since side effects due to acetazolamide were rarely observed, the present drug was considered to have a high safety margin.
Am J Psychiatry 1999 Apr;156(4):617-23 Minor physical anomalies, dermatoglyphic asymmetries, and cortisol levels in adolescents with schizotypal personality disorder. Weinstein DD, Diforio D, Schiffman J, Walker E, Bonsall R. “The schizotypal personality disorder group showed more minor physical anomalies and dermatoglyphic asymmetries than the normal comparison group and higher cortisol levels than both of the other groups.”
Am J Psychiatry 1992 Jan;149(1):57-61 Congenital malformations and structural developmental anomalies in groups at high risk for psychosis. McNeil TF, Blennow G, Lundberg L. “The inferred genetic risk for psychosis does not appear to be associated with greater rates of early somatic developmental anomalies, suggesting that early developmental anomalies do not represent an expression of genetic influence toward psychosis.”
Schizophr Bull 1984;10(2):204-32. Psychophysiological dysfunctions in the developmental course of schizophrenic disorders. Dawson ME, Nuechterlein KH. “Two electrodermal anomalies are identified in different subgroups of symptomatic patients: (1) an abnormally high sympathetic arousal and (2) an abnormal absence of skin conductance orienting responses to innocuous environmental stimuli.”
Behav Brain Res 2000 Jan;107(1-2):71-83. Changes in adult brain and behavior caused by neonatal limbic damage: implications for the etiology of schizophrenia. Hanlon FM, Sutherland RJ. .”This study contributes to our understanding of the pathogenesis of schizophrenia by showing that early damage to limbic structures produced behavioral, morphological, and neuropharmacological abnormalities related to pathology in adult schizophrenics.”
Neurochem Res 1996 Sep; 21(9):995-1004. Mitochondrial involvement in schizophrenia and other functional psychoses. Whatley SA, Curti D, Marchbanks RM. “Gene expression has been studied in post-mortem frontal cortex samples from patients who had suffered from schizophrenia and depressive illness.” “We conclude that changes in mitochondrial gene expression are involved in schizophrenia and probably other functional psychoses.”
Eur J Pharmacol 1994 Aug 11;261(1-2):25-32. The effect of alpha 2-adrenoceptor antagonists in isolated globally ischemic rat hearts. Sargent CA, Dzwonczyk S, Grover GJ. “The alpha 2-adrenoceptor antagonist, yohimbine, has been reported to protect hypoxic myocardium. Yohimbine has several other activities, including 5-HT receptor antagonism, at the concentrations at which protection was found.” “The cardioprotective effects of yohimbine were partially reversed by 30 microM 5-HT. These results indicate that the mechanism for the cardioprotective activity of yohimbine may involve 5-HT receptor antagonistic activity.”
J Cardiovasc Pharmacol 1993 Oct;22(4):664-672. Protective effect of serotonin (5-HT2) receptor antagonists in ischemic rat hearts. Grover GJ, Sargent CA, Dzwonczyk S, Normandin DE, Antonaccio MJ.
J Appl Physiol 1994 Jul;77(1):277-284. Aerobic muscle contraction impaired by serotonin-mediated vasoconstriction. Dora KA, Rattigan S, Colquhoun EQ, Clark MG.
J Cereb Blood Flow Metab 1995 Jul;15(4):706-13. Enhanced cerebrovascular responsiveness to hypercapnia following depletion of central serotonergic terminals. Kelly PA, Ritchie IM, McBean DE, Sharkey J, Olverman HJ.
Arch Gen Psychiatry 1984 Mar;41(3): 293-300. Regional brain glucose metabolism in chronic schizophrenia. A positron emission transaxial tomographic study. Farkas T, Wolf AP, Jaeger J, Brodie JD, Christman DR, Fowler JS. “. . . schizophrenics had significantly lower activity in the frontal lobes, relative to posterior regions.”
Semin Nucl Med 1986 Jan;16(1):2-34. Positron emission tomography imaging of regional cerebral glucose metabolism. Alavi A, Dann R, Chawluk J, Alavi J, Kushner M, Reivich M. “In patients with Alzheimer’s disease . . . parietal, temporal, and to some degree, frontal glucose metabolism is significantly diminished even in the early stages of the disease. Patients with Huntington’s disease and those at risk of developing this disorder have a typical pattern of diminished CMRglu in the caudate nuclei and putamen. In patients with stroke, PET images with FDG have demonstrated abnormal findings earlier than either XCT or MRI and with a wider topographic distribution. FDG scans have revealed interictal zones of decreased LCMRglu in approximately 70% of patients with partial epilepsy. The location of the area of hypometabolism corresponds to the site of the epileptic focus as determined by electroencephalography and microscopic examination of the resected tissue.”
Schizophr Bull 1988; 14(2): 169-76. From syndrome to illness: delineating the pathophysiology of schizophrenia with PET. Cohen RM, Semple WE, Gross M, Nordahl TE. “In normal controls, the metabolic rate in the middle prefrontal cortex, measured during the ongoing performance of auditory discrimination, is associated with their accuracy of performance. In unmedicated patients with schizophrenia, even those who performed as well as normals, the metabolic rate in the mid-prefrontal cortex was found to be significantly lower than normal. Further, this decreased metabolic rate was unrelated to performance.” “The mid-prefrontal cortex and its dopamine neurotransmitter pathway input are important biological determinants of sustained attention.”
Biol Psychiatry 1989 Apr 1;25(7):835-51. Increased temporal lobe glucose use in chronic schizophrenic patients. DeLisi LE, Buchsbaum MS, Holcomb HH, Langston KC, King AC, Kessler R, Pickar D, Carpenter WT Jr, Morihisa JM, Margolin R, et al. Temporal lobe glucose metabolic rate was assessed in 21 off-medication patients with schizophrenia and 19 normal controls by positron emission tomography with 18F-deoxyglucose. Patients with schizophrenia had significantly greater metabolic activity in the left than the right anterior temporal lobe, and the extent of this lateralization was in proportion to the severity of psychopathology.
Am J Obstet Gynecol 1999 Dec;181(6):1479-84. Stimulated nitric oxide release and nitric oxide sensitivity in forearm arterial vasculature during normotensive and preeclamptic pregnancy. Anumba DO, Ford GA, Boys RJ, Robson SC. “Alterations in serotonin receptor coupling to nitric oxide synthase, or a limitation of availability of the substrate for nitric oxide synthase (L-arginine) during pregnancy, could account for the reduction in stimulated nitric oxide release.”
J Hypertens 1999 Mar;17(3):389-96. U46619-mediated vasoconstriction of the fetal placental vasculature in vitro in normal and hypertensive pregnancies. Read MA, Leitch IM, Giles WB, Bisits AM, Boura AL, Walters WA.
Am J Obstet Gynecol 1999 Feb;180(2 Pt 1):371-7. Ketanserin versus dihydralazine in the management of severe early-onset preeclampsia: maternal outcome. Bolte AC, van Eyck J, Kanhai HH, Bruinse HW, van Geijn HP, Dekker GA. “Ketanserin [a selective serotonin 2 receptor blocker] is an attractive alternative in the management of severe early-onset preeclampsia.”
Am J Obstet Gynecol 1996 Dec;175(6):1543-50. Novel appearance of placental nuclear monoamine oxidase: biochemical and histochemical evidence for hyperserotonomic state in preeclampsia-eclampsia. Gujrati VR, Shanker K, Vrat S, Chandravati, Parmar SS. “Placental serotonin increases with severity (rsystolic 0.84, rdiastolic 0.83) and monoamine oxidase decreases (rsystolic 0.86, rdiastolic 0.79). Placental monoamine oxidase showed marked changes in preeclampsia-eclampsia.” .”A severity-dependent decrease was present in the nuclei of placentas with preeclampsia-eclampsia.” “The study delineates an impaired catabolism of placental serotonin in preeclampsia-eclampsia.” “The novel appearance of monoamine oxidase in nuclei in proximity to its normal site and low activity resulting in a hyperserotonomic state may lead to preeclampsia-eclampsia.”
Chung Hua Fu Chan Ko Tsa Chih 1996 Nov;31(11):670-2 [Changes of plasma levels of monoamines in normal pregnancy and pregnancy-induced hypertension women and their significance]. Lin B, Zhu S, Shao B. “Compared with NP [normal pregnant], the contents of DA in moderate and severe PIH [pregnancy-induced hypertension] were markedly and very markedly decreased respectively (P < 0.05 and P < 0.01), while the levels of 5-HT in PIH increased significantly (P < 0.05).” “The changes of monoamines may be one of the causes of small artery spasm in PIH.”
Lancet 1997 Nov 1;350(9087):1267-71. Randomised controlled trial of ketanserin and aspirin in prevention of pre-eclampsia. Steyn DW, Odendaal HJ. “Pre-eclampsia is associated with extensive endothelial-cell damage and platelet activation, resulting in lower production of vasodilator prostaglandins and increased release of the vasoconstrictors thromboxane A2 and serotonin.” “We investigated the role of ketanserin, a selective serotonin-2-receptor antagonist, in lowering the rate of pre-eclampsia among pregnant women with mild to moderate hypertension.” “There were significantly fewer cases of pre-eclampsia (two vs 13; relative risk 0.15 [95% CI 0.04-0.66], p = 0.006) and severe hypertension (six vs 17; p = 0.02) in the ketanserin than in the placebo group. There was also a trend towards less perinatal mortality (one vs six deaths) but this was not significant (p = 0.28). Rates of abruptio placentae and pre-eclampsia before 34 weeks’ gestation were lower in the ketanserin group, and mean birthweight was significantly higher.”
Osaka City Med J 1989 Jun;35(1):1-11. Serotonin and tryptamine metabolism in the acute hepatic failure model: changes in tryptophan and its metabolites in the liver, brain and kidney. Kodama C, Mizoguchi Y, Kawada N, Sakagami Y, Seki S, Kobayashi K, Morisawa S.
Br J Pharmacol 1984 Apr;81(4):645-650. Induction of hypoglycaemia and accumulation of 5-hydroxytryptamine in the liver after the injection of mitogenic substances into mice. Endo Y.
Eur J Pharmacol 1983 Aug 5;91(4):493-499. A lipopolysaccharide and concanavalin A induce variations of serotonin levels in mouse tissues. Endo Y.
Brain Res 1986 Jul 16;378(1):164-8 5-Hydroxytryptamine-2 antagonist increases human slow wave sleep. Idzikowski C, Mills FJ, Glennard R Ritanserin, a specific 5-HT2 antagonist, was given to volunteers in a double-blind placebo controlled sleep study. Slow wave sleep doubled in duration at the expense of stage 2. The finding that a serotonin antagonist changed the architecture of sleep without producing insomnia is of fundamental importance and calls for a re-examination of traditional theories of sleep control which assign a facilitatory role to serotonin.
Med Hypotheses 2000 Apr;54(4):645-7 Role of the pineal gland in hibernators: a concept proposed to clarify why hibernators have to leave torpor and sleep. Kocsard-Varo G.
Chronobiol Int 2000 Mar;17(2):103-28. The temporal organization of daily torpor and hibernation: circadian and circannual rhythms. Kortner G, Geiser F.
Neuroreport 2000 Mar 20;11(4):881-5 Slow waves in the sleep electroencephalogram after daily torpor are homeostatically regulated. Deboer T, Tobler I.
Neuroendocrinology 1982 Jun; 34(6): 438-443. Sleep organization in hypo- and hyperthyroid rats. Carpenter AC, Timiras PS. “The results show an increased number of awakenings during slow wave sleep (SWS) in hypothyroid animals, whereas total sleep time, levels of SWS, paradoxical sleep, and diurnal organization were unaffected by thyroid status. Our findings indicate that adequate levels of thyroid hormone are necessary to sustain extended periods of SWS in the adult rat while hyperthyroid animals show no disruption of sleep organization. A corollary finding is that daily sleep quotas are independent of whole body metabolic rates.”
© Ray Peat Ph.D. 2009. All Rights Reserved. www.RayPeat.com